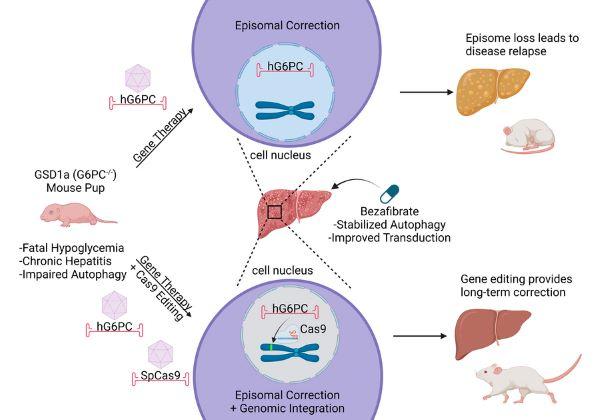
A study from Duke researchers in pediatrics and molecular genetics and microbiology shows that genome editing could be a promising and safe long-term treatment for infants with glycogen storage disease type Ia, a rare genetic condition that can lead to dangerously low blood sugar levels, especially in infants.
The disease impairs the liver’s ability to properly release sugar into the blood, and traditional gene therapy hasn’t worked well for treating it early in life.
Researchers led by Dwight Koeberl, MD, PhD, professor of pediatrics, professor of cell biology, and professor in molecular genetics and microbiology, tested a new approach using genome editing in baby mice with GSD Ia. They used two genetic tools delivered by modified viruses, called AAV vectors: one vector carried a gene to treat the disease, and the other vector carried the gene-editing tool CRISPR-Cas9, which helps insert that gene into the right spot in the chromosomal DNA.
They found that using both tools together — along with a drug called bezafibrate to improve the liver cells themselves — was effective. It prevented low blood sugar and improved survival. Importantly, the gene was successfully inserted into the DNA in a way that could help avoid long-term liver problems.
For safety, the researchers checked to make sure the CRISPR tool didn’t accidentally stay in the DNA, and it didn’t, which is an encouraging sign for future treatments.
The study is published online in JCI Insight.
The team aims to seek funding to further develop this method of genome editing with the goal of eventually launching a human clinical trial, Koeberl said.
Funding: The National Institutes of Health, the Alice and Y. T. Chen Center for Genetics and Genomics, Pfizer NC Biotechnology Gene Therapy Fellowship.